Additional Resources on Hypothyroidism
In this section, you will find educational modules that provide an overview of thyroid disorders, information on the thyroid and cardiovascular disease, and information on hypothyroidism during pregnancy. Also provided are answers to some frequently asked questions on the basics of hypothyroidism and related comorbidities.
Frequently Asked Questions Related to Hypothyroidism
Basics of Understanding Hypothyroidism
The thyroid gland produces two major hormones: thyroxine (T4) and triiodothyronine (T3). Secretion of these hormones is triggered by thyroid-stimulating hormone (TSH), which is made by the pituitary gland.1 Thyroid hormones control metabolism and have a profound effect on a wide range of physiologic functions including regulation of body temperature, muscle strength, body weight, lipid levels, and neurological, respiratory, and cardiovascular functions.1,2
Thyroid disorders can generally be classified as those resulting either from overproduction or underproduction of thyroid hormones by the thyroid gland. Primary hypothyroidism refers to hormone deficiency caused by intrinsic dysfunction of the thyroid gland that disrupts the synthesis and secretion of T4 and T3. Secondary or tertiary hypothyroidism, also called central hypothyroidism, refers to deficient thyroid gland function that is the result of inadequate stimulation by thyroid-stimulating hormone (TSH). This is due, in turn, to insufficient or ineffective production of TSH because of pituitary or hypothalamic disorders.1,2 Primary hypothyroidism is common and accounts for majority of cases of hypothyroid disease whereas central hypothyroidism is rare, representing less than 1% of cases.1,2
Hyperthyroidism develops when there is excessive synthesis and secretion of thyroid hormones from the thyroid gland. The most common cause of hyperthyroidism is Graves’ disease, in which thyroid-stimulating immunoglobulins (autoantibodies) bind to and activate the TSH receptor, promoting thyroid hormone secretion and growth of the thyroid gland.2
Hyperthyroidism develops when there is excessive synthesis and secretion of thyroid hormones from the thyroid gland. The most common cause of hyperthyroidism is Graves’ disease, in which thyroid-stimulating immunoglobulins (autoantibodies) bind to and activate the TSH receptor, promoting thyroid hormone secretion and growth of the thyroid gland.2
Most cases of hypothyroidism in the developed world result from primary thyroid failure due to chronic autoimmune inflammation of the thyroid gland and destruction of thyroid tissue (Hashimoto’s thyroiditis). Other causes include congenital absence of thyroid tissue, radioactive iodine therapy (ie, for Graves’ disease, nodular goiter, or thyroid cancer), surgical removal of all or part of the thyroid, infiltrative destruction of thyroid tissue (ie, hemochromatosis, scleroderma, or amyloidosis), iodine imbalance in the thyroid, nutritional iodine deficiency, and certain medications that interfere with thyroid hormone production or release (ie, thionamides, amiodarone, lithium).1,2
Some of the common risk factors for developing hypothyroidism include a family history of thyroid diseases, older age, female gender, presence of other autoimmune diseases (ie, type 1 diabetes, Sjögren’s syndrome, celiac disease, vitiligo), and goiter.1,2
The signs and symptoms associated with hypothyroidism vary according to age at onset, disease severity, and rapidity with which the disease occurs. Common symptoms of hypothyroidism are nonspecific in nature, which may make it difficult to recognize hypothyroidism.1,2
Signs and symptoms of hypothyroidism include1,2:
Signs and symptoms of hypothyroidism include1,2:
- Fatigue, weakness, lethargy
- Weight gain
- Cold intolerance
- Dry, rough, thick skin
- Coarseness of hair
- Brittle nails
- Depressed mood, limited sociability
- Hoarseness of voice
- Slowed speech and movement
- Delayed reflexes
- Cognitive defects
- Constipation
- Bradycardia
- Diastolic hypertension
- Arthralgia
- Myalgia
- Menstrual irregularity
Measurement of serum thyroid-stimulating hormone (TSH) is the primary screening test for thyroid dysfunction. The American Association of Clinical Endocrinologists and American Thyroid Association clinical practice guidelines indicate that the normal range for serum TSH should be between 0.45 mIU/L (lower limit of normal) and 4.12 mIU/L (upper limit of normal).3 Elevated serum TSH and subnormal serum free T4 (FT4) levels establish a diagnosis of primary hypothyroidism.3
Hypothyroidism may manifest as either clinical (overt) or subclinical. Overt hypothyroidism is characterized by an elevated serum thyroid-stimulating hormone (TSH), in combination with a subnormal free T4 (FT4). Patients with overt hypothyroidism often have TSH levels above 10 mlU/L. Subclinical hypothyroidism is characterized by elevated serum TSH levels but normal FT4.3 Target serum TSH value is typically 0.45-4.12 mIU/L, but varies depending on patient factors such as patient’s age, comorbidities, and population norms.
References
- Pellitteri PK, Ing S, Jameson B. Disorders of the thyroid gland. In: Flint: Cummings Otolaryngology: Head & Neck Surgery, 5th ed. 2010;1735-1749.
- Kim M and Ladenson P. Goldman: Goldman's Cecil Medicine, 24th ed. 2011:e64-e77.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: co-sponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18(6).
Hypothyroidism and Comorbidities
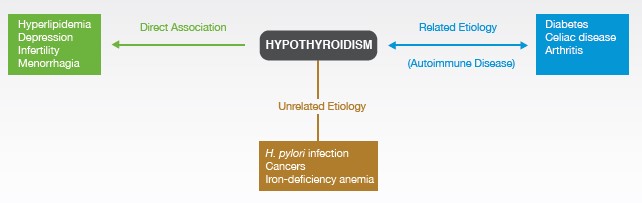
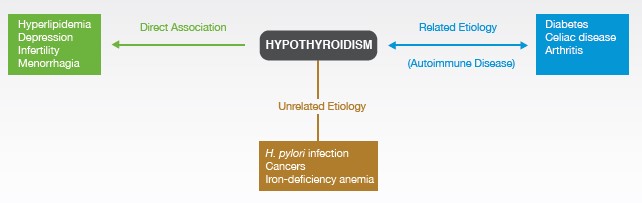
Hypothyroidism is etiologically associated with multiple comorbidities, some are caused by the hypothyroidism itself, while others are related in etiologic origin. Comorbidities of hypothyroidism such as hyperlipidemia, depression, menorrhagia, and fertility problems are thought to result from hypothyroidism itself. A number of autoimmune diseases such as type 1 diabetes mellitus (T1DM), celiac disease, and rheumatoid arthritis are not caused by hypothyroidism, but they share a related etiology. Certain other diseases are not etiologically linked but may affect coexisting hypothyroidism.
Thyroid hormones exert a regulatory influence over the cardiovascular system. Hypothyroidism reduces myocardial contractility and heart rate, leading to reductions in cardiac output and exercise tolerance as well as increases in systemic vascular resistance and diastolic blood pressure.1,2 Patients with hypothyroidism may also present with pericardial and pleural effusions, which may account for the low voltage seen on electrocardiographic tracings of these individuals.2 In addition, rising TSH levels, particularly concentrations of 10 mIU/L or greater, are associated with increased risk of coronary heart disease (CHD) mortality and CHD events.3
Thyroid disorders, including overt hypothyroidism and subclinical hypothyroidism, considerably alter the lipid profile, which may in turn promote cardiovascular disease. Hypothyroidism results in reduced expression of low-density lipoprotein (LDL) receptors and is associated with increased biliary excretion of cholesterol and uptake of cholesterol from the circulation by the liver.4 Although the prevalence of overt hypothyroidism in patients with hypercholesterolemia is estimated to be 1.3%-2.8%, 90% of patients with hypothyroidism have been found to have hypercholesterolemia.1
A body of clinical case reports, epidemiological studies, biochemical observations, and case control and cohort studies have linked hypothyroidism and atherosclerosis. One study found that coronary artery atherosclerosis is twice as common in patients with hypothyroidism compared with sex- and age-matched controls.5
A body of clinical case reports, epidemiological studies, biochemical observations, and case control and cohort studies have linked hypothyroidism and atherosclerosis. One study found that coronary artery atherosclerosis is twice as common in patients with hypothyroidism compared with sex- and age-matched controls.5
Type 1 diabetes mellitus (T1DM) has a higher prevalence in patients with autoimmune thyroid disease than in the general population due to the related autoimmune origins of the conditions. Chronic thyroiditis develops in about 10% of T1DM patients,6 and about 3%-8% of children and adolescents with T1DM have been reported to develop autoimmune hypothyroidism.7 In addition, postpartum thyroiditis will develop in up to 25% of women with T1DM.6 The prevalence of type 2 diabetes mellitus (T2DM) in patients with hypothyroidism is similar to that of the general population.
The American Association of Clinical Endocrinologists and American Thyroid Association guidelines recommend that the diagnosis of overt or subclinical hypothyroidism must be considered in every patient with depression.6 A small proportion of all patients with depression have primary hypothyroidism.
Overt untreated hypothyroidism during pregnancy may adversely affect maternal and fetal outcomes. These adverse outcomes include increased incidences of spontaneous miscarriage, preterm delivery, preeclampsia, maternal hypertension, postpartum hemorrhage, low birth weight and stillbirth, and impaired intellectual and psychomotor development of the fetus.6
Universal screening for hypothyroidism is not recommended preconception or during pregnancy.8 However, it is strongly suggested that healthcare professionals personally ask about a patient’s risk factors for thyroid disease during preconception counseling or the first obstetric visit. Thyroid-stimulating hormone (TSH) testing should be conducted in women seeking pregnancy or early in pregnancy who are at high risk for developing hypothyroidism.8 Risk factors include women with a history of pregnancy loss, preterm delivery, or infertility or those who have had multiple prior pregnancies.
During pregnancy, serum thyroid-stimulating hormone (TSH) levels decline in the first trimester when serum human chorionic gonadotropin levels are high and rise after 10-12 weeks of gestation.6 According to the new American Thyroid Association guidelines, maternal hypothyroidism is defined as a TSH concentration elevated beyond the upper limit of the pregnancy- and population-specific reference ranges.8 However, recognizing that this may not always be feasible, an upper reference limit of 4.0 mIU/L is recommended.8
References
- Klein I and Danzi S. Thyroid disease and the heart. Circulation. 2007;116:1725-1735.
- Devdhar M, Ousman YH, Burman KD. Hypothyroidism. Endocrinol Metab Clin N Am. 2007;36(3):595-615.
- Rodondi N, den Elzen WP, Bauer DC, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304(12):1365-1374.
- Duntas LH, Brenta G. The effect of thyroid disorders on lipid levels and metabolism. Med Clin North Am. 2012;96:269-281.
- Squizzato A, Gerdes VE, Brandjes DP, Buller HR, Stam J. Thyroid diseases and cerebrovascular disease. Stroke. 2005;36:2302-2310.
- Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: co-sponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18(6).
- Brenta G. Diabetes and thyroid disorders. Br J Diabetes Vasc Dis. 2010;10:172-177.
- Alexander EK, Pearce EN, Brent GA, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017;27(3):315-389. doi:10.1089/thy.2016.0457
ABBV-US-00119-MC V1.0
02/2020
02/2020